PCMA Statement Ahead Of House Suspension Vote
(Washington, D.C.) — The Pharmaceutical Care Management Association (PCMA) released the following statement today ahead of next week’s U.S. House of Representatives suspension vote on the Lower Costs, More Transparency Act.
“Next week, House Leadership is scheduled to bring the Lower Costs, More Transparency Act up for a vote under suspension of the rules. If passed, this measure would represent an unprecedented overreach by Congress to interfere with private market contracting for pharmacy benefits. Preserving options for employers, especially smaller self-insured employers, to choose how best to contract with their pharmacy benefit company, allows employers to make choices that best meet their goals and unique healthcare needs when providing pharmacy benefits to their employees.
“To be clear, PBMs fully support transparency for health plans, employers and patients. Unfortunately, this legislation would give drug companies competitive information leading to lower discounts and higher prescription drug costs for everyone.
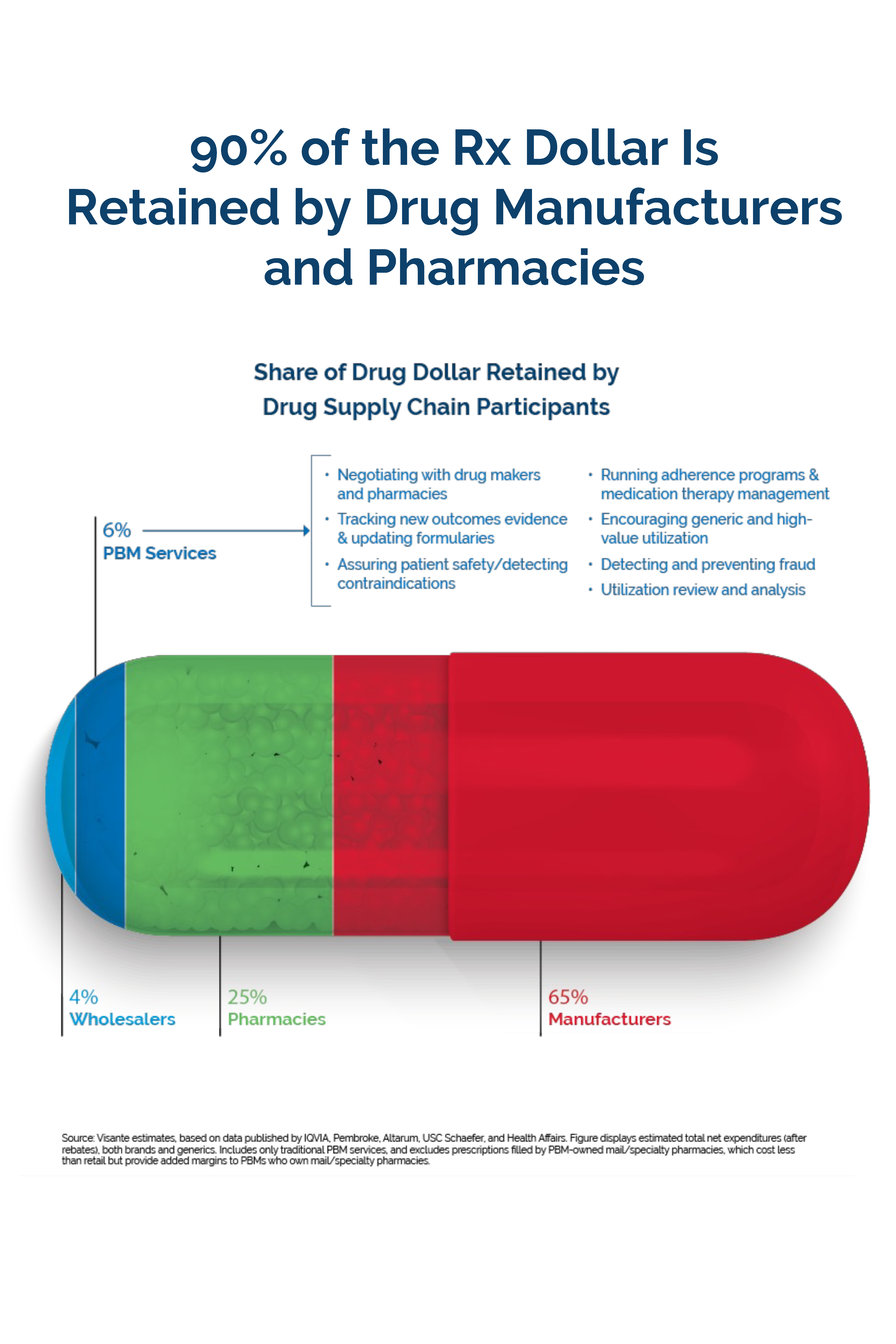
“It is unclear what problem the legislation is attempting to solve when it explicitly does nothing to lower prescription drug costs for employers and patients, and focuses only on PBMs, ignoring all the other actors in the supply chain. To be clear, PBMs fully support transparency for health plans, employers, and patients. Unfortunately, this legislation would give drug companies competitive information leading to lower discounts and higher prescription drug costs for everyone.
“Further, the legislation should be deemed completely unnecessary in light of the new and innovative pharmacy benefit design choices PBMs are bringing to the market so that employers have the flexibility to choose the type of plan and what types of transparency disclosures work best for them and their enrollees.”
Survey Finds Overwhelming Majority of Employers Value a Wide Range of Pharmacy Benefit Company Contract Options
The Coalition for Affordable Prescription Drugs (CAPD), an organization that represents a diverse group of public and private stakeholders, released a survey that found an overwhelming majority of employers value their pharmacy benefit company. The survey included more than 700 employers across the country with 50+ employees who offer prescription drug benefits to employees.
Key findings from the survey include:
- 89 percent of employers say their PBM is valuable in helping their organization offer affordable benefits to employees.
- 93 percent of employers say it is essential to have flexibility and a range of choices in how they offer prescription drug benefits to employees, with 86 percent of employers saying it is important to have a range of options in how they pay PBMs for their services and expertise.
- The same number (86 percent) say it is important to have flexibility in how their organization manages the financial risk related to prescription drug spending. Nearly one third of employers choose to manage that risk and compensate their PBM through “spread” or risk-mitigation/predictable pricing.
- 89 percent of employers who use a PBM describe their contract as transparent, with 43 percent describing their contract as “very transparent.”
View the CAPD Survey HERE.